Health


KUWAIT: In the relentless pursuit of rapid weight loss, many individuals have turned to using diabetic shots to shed pounds quickly. This trend has gained significant traction, with the practice becoming increasingly widespread. However, the safety and efficacy of such methods remain subjects of concern, as the risks and potential side effects associated with using diabetic shots for weight loss are not yet fully understood.
Kuwait Times spoke with several people who use diabetic shots as a weight loss strategy. Sahar Moussa, 46, embarked on her journey with Ozempic twice. The first time was two years ago, when she diligently adhered to a regimen of the medication for three consecutive months. Her decision to take Ozempic was influenced by its affordability, as it offered a viable solution to her weight management concerns.
“The dosage entailed a gradual escalation, starting with 0.5 milligrams administered once weekly for a month, followed by increments to 1.5 milligrams in the second month and up to 2 milligrams in the third,” she explained. Despite experiencing initial side effects such as nausea, headaches, and fatigue, Moussa persisted, driven by her determination to combat cravings, particularly for sweets, leading to losing nine kilograms over three months.
However, the unavailability of Ozempic in Kuwait at the time and its resulting hefty price tag of KD 50 prompted her to discontinue its usage, confident in her ability to maintain her progress independently. But after two months, Moussa found herself grappling with the unwelcome return of weight, swiftly regaining 7 kg and reaching a weight of 78 kg.
The second usage of Ozempic was unplanned. It started when Moussa’s uncle lacked success with his medication (Ozempic) for his diabetes management, so he gave her his shot to try losing weight again. She is now re-embarking on her weight loss journey, determined to reclaim control over her eating habits and achieve her desired goals.
As for Nasser Hussain, 33, he used the Mounjaro diabetic shot 11 months ago, arguing the shot is certified by the World Health Organization for weight loss and he felt safe to use it in his weight loss journey. Hussein paid KD 150 per injection, affirming that it was worth it, as he lost 32 kg in five months. Regarding side effects, he had a mild headache and backache due to shrinking muscles, which he fixed with light exercise.
Hussain advised people to consult a doctor. “I consulted a doctor before getting into the process. In addition, I did several tests such as CBC, LFT, RFT + serum electrolyte, lipid profile, TFT and vitamin D,” he detailed. He called on people to take care of their health during the process by taking vitamins and not exhaust themselves too much to not suffer dizziness from low blood sugar.
For his part, Khaled Al-Sharqawi used Saxenda, which he received as a gift from a friend who wanted to help him in his weight loss journey. “I started in January this year, and it was my first time to use diabetic medication for weight loss,” he said. Remarkably, within three months, Sharqawi successfully shed an impressive 15 kg, a testament to his dedication and the efficacy of the medication. Unlike some users who experience adverse effects, Khaled was fortunate to remain unaffected by any notable side effects.
However, he did observe a decrease in his daily food intake, a positive indication of the medication’s impact on his appetite control. Despite this reduction, the craving for sweets, particularly during nighttime, posed a lingering challenge. Adhering diligently to the instructions provided on the medication packaging, Sharqawi ensured consistent administration by injecting Saxenda once daily at the same time each day. Additionally, he maintained discipline in scheduling his meals, aligning them with the designated times recommended for optimal results. (Kuwait Times)
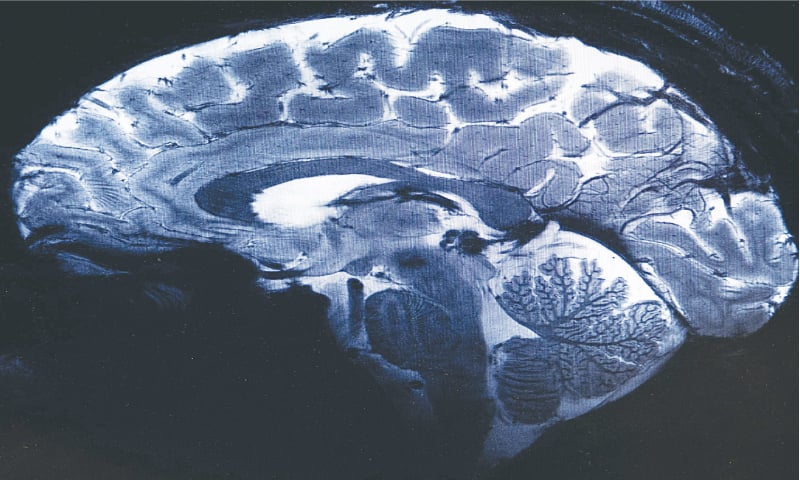
SACLAY: The world’s most powerful MRI scanner has delivered its first images of human brains, reaching a new level of precision that is hoped will shed more light on our mysterious minds — and the illnesses that haunt them.
Researchers at France’s Atomic Energy Commission (CEA) first used the machine to scan a pumpkin back in 2021. But health authorities recently gave them the green light to scan humans.
Over the past few months, around 20 healthy volunteers have become the first to enter the maw of the magnetic resonance imaging (MRI) machine, which is located in the Plateau de Saclay area south of Paris, home to many technology companies and universities.
“We have seen a level of precision never reached before at CEA,” said Alexandre Vignaud, a physicist working on the project. The magnetic field created by the scanner is a whopping 11.7 teslas, a unit of measurement named after inventor Nikola Tesla.
This power allows the machine to scan images with 10 times more precision than the MRIs commonly used in hospitals, whose power does not normally exceed three teslas. On a computer screen, Vignaud compared images taken by this mighty scanner, dubbed Iseult, with those from a normal MRI.

The mystery of so-called Havana Syndrome, which struck down dozens of US diplomats, deepened Monday as new research found no tangible evidence of brain injury in those affected. Researchers at the National Institutes of Health (NIH) acknowledged that ongoing symptoms including migraines, chronic dizziness, and depression are still very much real—even if they cannot yet be explained.
Havana Syndrome first baffled officials in 2016 when US diplomats in Cuba’s capital reported falling ill and hearing piercing sounds at night, sparking speculation of an attack by a foreign enemy using an unspecified sonar weapon. Similar reports of the illness later emerged from embassy staff in China, Europe and US capital Washington.
Yet despite the “disabling” symptoms, people with Havana Syndrome—formally referred to as anomalous health incidents (AHIs) -- show no clinical differences, according to two new papers published Monday in peer-reviewed journal JAMA.
Leighton Chan, lead author of one of the papers, said “it’s important to acknowledge that these symptoms are very real, cause significant disruption in the lives of those affected and can be quite prolonged, disabling and difficult to treat.” In this study, researchers assessed more than 80 US government officials and their family members using MRI brain scans and other blood, visual and auditory tests. They were compared with a control group of overseas US officials who had similar work assignments but were unaffected by the symptoms. It found those with AHIs self-reported increased symptoms of fatigue, post-traumatic stress and depression.
Forty one percent of those with AHIs met the criteria for “functional neurological disorder”—problems with the way the brain sends and receives information from the rest of the body, and as a result nearly all with this dysfunction could be diagnosed with a chronic form of dizziness. “These individuals have symptoms that are genuine, distressing, and can be quite prolonged, disabling, and difficult to treat,” said the researchers.
In the second paper, participants underwent MRI scans to examine their brain size, structure, and function. These were carried out on average 80 days after symptom onset and revealed no imaging abnormalities differentiating the group with AHIs. But this “does not exclude that an adverse event impacting the brain occurred at the time of the AHI,” said Carlo Pierpaoli, who led the study.
The US State Department was reviewing the research, a spokesperson said Monday, adding its “top priority remains the health, safety, and security of the Department’s personnel and family members.” US intelligence had said in 2022 that intense directed energy from an external source could have caused some cases of Havana Syndrome, officially known as anomalous health incidents (AHIs).
But in March 2023 intelligence agencies concluded that “there is no credible evidence that a foreign adversary has a weapon or collection device that is causing AHIs.” They reported the symptoms were probably the result of preexisting conditions, conventional illnesses and environmental factors.
David Relman of Stanford University, who has led previous research into Havana, said the new study was flawed as not all brain injuries were detectable with the tests used. In an editorial also published in JAMA, Relman cited two previous studies he contributed to which found the cases “to be unlike any disorder reported in the neurological or general medical literature, and potentially caused by an external mechanism.”—AFP

Drugmaker AstraZeneca (AZN.L), opens new tab said on Thursday it would acquire rare endocrine diseases-focused firm Amolyt Pharma for $1.05 billion in cash, in a bid to boost its rare diseases portfolio.
Amolyt, backed by investors including Danish drugmaker Novo Nordisk's (NOVOb.CO), opens new tab parent firm Novo Holdings and EQT Life Sciences, is currently in the late-stage development of a therapy for hypoparathyroidism.
The deal, which includes an $800 million upfront payment and additional contingent payment of $250 million on achieving a specified regulatory milestone, is expected to close by the third quarter of 2024.
Advertisement · Scroll to continue
In almost a decade since AstraZeneca fended off a takeover by U.S. rival Pfizer (PFE.N), opens new tab, CEO Pascal Soriot has rebuilt the Anglo-Swedish drugmaker's pipeline, which includes 13 blockbuster medicines - those that generate more than $1 billion in annual sales.
Last month, Soriot said it was a "good time" for the company to do deals. The deal for Amolyt comes amid a string of acquisitions including a licensing deal late last year that gave AstraZeneca an entry into the booming anti-obesity drug market.
Advertisement · Scroll to continue
Revenue from the company's rare diseases portfolio, boosted by the $39 billion acquisition of Alexion in 2021, have also swelled in recent years, clocking nearly $7.8 billion in 2023. (Reuters)

More than 1 billion peopleTrusted Source globally have at least one migraine attack each year.
Previous studies show that migraine can potentially increase a person’s risk for other conditions, including strokeTrusted Source, heart diseaseTrusted Source, epilepsyTrusted Source, sleeping issuesTrusted Source, and anxiety and depressionTrusted Source.
Migraine has also been linked to some gastrointestinal conditionsTrusted Source, including irritable bowel syndrome (IBS)Trusted Source.
Now, researchers from Seoul National University College of Medicine in South Korea say there may also be a link between migraine and an increased risk for irritable bowel disease (IBD), which is an umbrella term that includes Crohn’s disease and ulcerative colitis.
The study was recently published in the journal Scientific ReportsTrusted Source.
Migraine and IBD: An unsurprising connection
According to Dr. Brooks D. Cash, professor and chief of the division of Gastroenterology, Hepatology, and Nutrition at UTHealth Houston in Texas, who was not involved in this study, the field of gastroenterology has recognized for many years that migraine has been associated with many chronic gastrointestinal syndromes and diseases.
“The data in this report supports previous reports of an association between migraine headaches and IBD,” Dr. Cash told Medical News Today.
Dr. Rudolph Bedford, a board-certified gastroenterologist at Providence Saint John’s Health Center in Santa Monica, CA, who was also not involved in this study, told MNT that the research results were not surprising.
“[With] inflammatory bowel disease we do see some extra-intestinal manifestations including things involving the eye or ocular findings, which may be neurogenic in nature, so it wasn’t surprising,” Dr. Bedford added.
This is not the first study to look at a connection between migraine and IBD.
A study published in March 2021 of people in the United States found a higher prevalenceTrusted Source of migraine or severe headaches among adults with IBD than in those without.
Research published in March 2023 reported an increased prevalence of IBD in people with migraine with and without aura.
Could migraine increase risk of inflammatory bowel disease?
For the current study, researchers analyzed data from more than 10 million people through the nationwide healthcare system for South Korean citizens. About 3% of the study population had IBD.
Through the data, scientists found the incidence of IBD was significantly higher in people who had migraine compared to those who did not.
Scientists also reviewed the data through subgroups of Crohn’s disease and ulcerative colitis incidences. People with migraine in both subgroups had a higher risk of developing either condition when compared to people without migraine.
After a migraine diagnosis, researchers found people were at a higher risk of developing Crohn’s disease, with a significant rise after a 5-year follow-up.
Additionally, within the subgroups, scientists reported that the impact of migraine on the risk of developing ulcerative colitis was more prominent in men than women.
Study results not definitive
Based on these findings, the research team suggests that people with migraine be monitored carefully for the development of IBD.
However, Dr. Cash stated that the data presented do not convincingly support that approach or recommendation.
“The odds ratios that were reported in this study, which can be thought of as the increased odds of an outcome (e.g., developing IBD) with a given exposure (e.g., migraine headaches), were consistently between one to two, which is not far from definitive and can be easily misinterpreted or misrepresented,” he explained.
“The results are, at best, suggestive of an association between migraines and IBD, which we were already aware of based on previous research and deserve to be further evaluated. However, the minimal increase in the odds of developing IBD reported in this study is not sufficient to recommend increased monitoring of patients with migraines for the development of Crohn’s disease or ulcerative colitis.”
– Dr. Brooks D. Cash
Importance of identifying potential IBD triggers
Dr. Bedford said it is important to identify potential health issues that may trigger IBD, as a doctor may be able to mitigate the symptoms of IBD if they know what may be associated with it.
“Migraines can be very debilitating and you may want to identify those people with migraines,” he continued. “We don’t normally question patients with inflammatory bowel disease whether or not they have migraine headaches, so it probably rates as something that should be done more frequently.”
“These results add to an already relatively robust body of research suggesting that chronic pain syndromes are statistically more common in patients with chronic GI syndromes or diseases,” Dr. Cash said.
“We do not have enough information or proof yet to establish a causal relationship either way. But this data can be used to explain some therapeutic approaches that may benefit both GI and neurologic symptoms in patients with migraines,” he added.
Research next steps
Regarding the next steps for this research, Dr. Cash said that mechanistic data evaluating the possible reasons for these consistent observations of association is needed.
“Right now, all we have are hypotheses,” he continued. “Are there changes in the gut-brain communication pathways or sensory perceptions in the enteric and central nervous systems? Is the gut microbiome involved? Are there psychological and stress-mediated factors at play?”
“Once clinical relationships such as these have been identified, we need to move toward trying to explain why those relationships may exist,” Dr. Cash added. “That, in turn, may lead us to develop more targeted and effective therapies that can address multiple symptoms/syndromes.”
Dr. Bedford suggested researchers look for an association between IBD flares and migraine occurring at the same time. As migraine is associated with serotonin release, he encouraged researchers to examine how the serotonin transporters within the GI tract, small bowel, and colon might play a role.
“I think just questioning our patients in terms of quality of life issues — is there any way that we can mitigate their migraine headaches, potentially preventing their inflammatory bowel disease flare, or vice versa, is certainly something to look into,” Dr. Bedford said.

Cases of the flu have fallen considerably since they peaked at the end of December, but they still remain elevated across the country. Will there be a second wave?
The latest trends from the Centers for Disease Control and PreventionTrusted Source show that cases of the flu appear to have leveled off rather than continue their downward trajectory. Lab-positive cases of the flu, one of several indicators that the CDC uses to assess seasonal influenza activity, are stable after trending upward last week. Meanwhile, other key indicators like flu-related hospitalizations and visits to healthcare providers are similar to weeks prior.
“We’re not out of the flu woods yet,” said Dr. William Schaffner, a Professor of Infectious Disease and Preventive Medicine at Vanderbilt University.
“There’s still plenty of flu out there and the anticipation is, as per usual, we will have flu through February and then it will really begin to taper during March,” he told Healthline.
Of course, flu isn’t the only respiratory illness circulating right now either. COVID-19 and respiratory syncytial virus infection (RSV)Trusted Source are still highly active as well. According to the latest CDC numbers, there have been more than 133,000 emergency department visitsTrusted Source nationally due to these three combined. Influenza is still the greatest driver, though, causing roughly 79,000 of those emergency room visits.
Is this flu season worse than other years?
There’s good reason to expect another bump in flu cases this year. Historically, influenza activity most often peaks in FebruaryTrusted Source, before finally falling off.
“I don’t have a great crystal ball, but it wouldn’t surprise me if we saw fairly high case numbers through mid-March,” said Dr. Dean Winslow, a Professor of Medicine at Stanford Medicine and infectious disease expert.
The 2023-2024 flu season has also been one of the most robust since the COVID-19 pandemic in 2019-2020.
Last year’s flu season was also strong, but it peaked much earlierTrusted Source, at the end of November, before crashing precipitously in December and January.
This year, the season appears to have peaked in the last week of December.
Right now flu cases are much higher than at the same time last year.
“In general, the country has seen a diminution in new cases of influenza, but it’s still way above the annual epidemic level. Our influenza cases are down somewhat, but they’re on a plateau, basically. They’re maintaining themselves,” said Schaffner.
Where are flu cases concentrated this week?
Monitoring the extent and severity of flu season is complex.
There are also important regional variations in flu activity across the United States. Southern states including Texas, New Mexico, Arkansas, Louisiana, and South Carolina are all showing very high levels of flu activity. Meanwhile, many western states, from Colorado to Oregon show moderate to low levels.
In order to establish what a national snapshot looks like, scientists at the CDC have to use a variety of indicators.
For example, this week the number of laboratory-confirmed positive influenzaTrusted Source cases sits at 15.8%. Out of more than 96,000 tested specimens, about 15,000 of them tested positive for the flu. The percentage of laboratory-confirmed tests has also been relatively stable for the past several weeks.
Another indicator, reported flu-related doctor visits, is at 4.4%. That means that out of all cases reported through one of the CDC’s respiratory illness surveillance programs, 4.4% met the definition of an “influenza-like illness” or ILITrusted Source. An ILI is defined as a fever of 100 degrees or more, accompanied by cough and/or sore throat.
Deaths due to the flu have also been falling in recent weeks. There were 222 flu-related deaths in the past week, compared to 490 the week before.
What to know about different flu strains
Like all viruses, the flu is prone to mutation, meaning that one flu season will differ from the next in terms of severity of symptoms and transmissibility. While there are four types of influenza viruses (A, B, C, and D), the first two are responsible for the annual flu seasonTrusted Source epidemic in the United States.
Influenza A makes up the bulk of cases year after year, while influenza B makes up a much smaller proportion of illnesses.
“There’s an old adage, if you’ve seen one flu season, you’ve seen one flu season. It’s usually the case that influenza B plays a minor role earlier in the annual outbreak and then becomes more prominent as we get through February into March,” said Schaffner.
This year’s virus, “influenza A(H1N1)pdm09,” might sound familiar to some readers. That H1N1 designation is one you’ve seen before.
“This particular strain of flu is very similar to the H1N1 virus which caused the catastrophic ‘Spanish Flu’ pandemic of 1918-19,” said Winslow.
“Interestingly, during the 1918-19 Spanish flu, a lot of cases were seen late in the season also,” he added.
H1N1 is a swine flu subtype of influenza A virus that, in addition to the famous 1918 pandemic, was also responsible for an outbreak in 2009-2010.Trusted Source At that time, it is estimated that the virus was responsible for somewhere between 43-89 million cases across 178 countries.
How to avoid catching the flu
The number one thing you can do to stay well during this flu season is to get a flu shot. Both Winslow and Schaffner recommend getting one, especially if you fall into a high-risk category.Trusted Source Individuals who are 65 years of age or older, children younger than 5, pregnant, or have certain chronic conditions are considered at higher risk from flu-related symptoms.
Other important considerations for staying well include minimizing time spent in large groups indoors and social distancing.
The bottom line
Flu season isn’t over yet. Cases are overall down from their peak at the end of December but are still considerably elevated nationally.
Cases have plateaued, but February is historically one of the peaks of flu season, and there is the potential for another wave.
Experts recommend getting a flu shot, avoiding large indoor group activities, and social distancing to stay safe from the flu this season.

Aerobic exercise is known to help the heart and the cardiovascular system. But now a new study finds that the exercise of tai chi may be a better option for people looking to lower their blood pressure.
According to the new study, tai chi proved to be more effective than aerobic exercise in lowering blood pressure among patients with prehypertension.
The findings were published February 9 in JAMA Network Open.Trusted Source
How to tell if you have high blood pressure
A blood pressure reading Trusted Sourceis comprised of two numbers. The top number is the systolic pressure or the pressure in your arteries when your heart beats. The bottom number is the diastolic pressure or the pressure in your arteries when your heart rests between beats.
A normal blood pressure level is less than 120 systolic over less than 80 diastolic (less than 120/80 mm Hg).
Prehypertension blood pressure is defined in this study as a systolic reading between 120-129 mm Hg and a diastolic pressure of 80-89 mm Hg.
High blood pressure levels or hypertension would be a systolic reading of 140 mm Hg or higher and a diastolic reading of 90 mm Hg or higher.
People taking tai chi saw larger drop in blood pressure
Researchers analyzed 342 participants with prehypertension between the ages of 18 and 65. Participants were placed in two groups. One group performed four 60-minute sessions of tai chi each week for one year. The other group performed the same number and frequency of sessions for aerobic exercise. The duration of the study was 2 and a half years.
“The study’s strengths lie in its robust methodology, including its prospective, single-blinded randomized clinical trial design,” said Dr. Joseph Daibes, cardiologist at Northwell Lenox Hill Hospital. “Randomized controlled trials are considered the gold standard for assessing the effectiveness of interventions as they minimize bias and allow for causal inference. The inclusion of a large sample size and its 12-month duration further enhances the reliability of the findings, providing a comprehensive assessment of the long-term effects of tai chi and aerobic exercise on blood pressure management.”
At the end of one year, there was a significant change in systolic blood pressure for both groups but a bigger drop in the tai chi group.
The researchers found an average systolic blood pressure change of −7.01 mm Hg in the tai chi group vs −4.61 mm Hg in the aerobic exercise group.
Daibes continued: “The study’s findings indicating that tai chi was more effective than aerobic exercise in reducing [systolic blood pressure] among individuals with prehypertension offer valuable insights for healthcare providers and patients alike. Tai chi, as a mind-body exercise, may offer unique benefits beyond traditional aerobic activities, such as stress reduction, improved relaxation, and enhanced mental focus, which could contribute to its superior efficacy in lowering blood pressure.”
Tai chi can help with anxiety, depression, and sleep issues
Growing evidence demonstrates the mental and physical benefits of tai chi, which include reducing anxiety and depression, improving sleep and cognitive performance, and promoting heart health.
“Tai chi exercise is characterized by slow, purposeful movements,” Joe Petreycik, RN, and physiotherapist, Bridgeport Hospital, explained. “It involves meditative breathing, mindfulness, and imagery. With meditation and imagery accepted as effective stress reduction techniques which can lower blood pressure, it makes sense that tai chi exercise would have similar blood pressure lowering benefits.”
In short, tai chi seems to have an advantage when it comes to lowering blood pressure in people dealing with prehypertension. This exercise primarily focuses on the mind-body connection.
“The slow, deliberate movements combined with focused breathing create a serene environment that’s perfect for dialing down stress levels – a big win for blood pressure management,” said Daibes.
Also, tai chi is extremely gentle on the body, making it accessible to most people.
“It’s not like your typical high-intensity workouts; it’s more like a peaceful dance that’s good for the soul,” Daibes explained. “And the benefits don’t stop there – tai chi also works wonders for circulation and cardiovascular health, which are key players in keeping blood pressure in check. With its holistic approach to wellness, tackling both physical and mental well-being, tai chi is shaping up to be a game-changer for folks looking to get a handle on their blood pressure.”
The health benefits of tai chi
Tai chi can improve your health in numerous ways, according to Dr. John Higgins, professor and sports cardiologist with UTHealth Houston. These include:
Lowering stress and blood pressure
Improving muscle strength
Improving balance and flexibility
Improving joint health
Improving sleep quality
Increasing bone density
Boosting the immune system
Improved lung function
Reduced cardiovascular disease
“Tai chi can certainly be helpful in improving exercise tolerance, particularly in those with barriers to regular aerobic exercise,” Petreycik stated.
Its gentle yet disciplined movements help improve balance, flexibility, and joint health, making it a popular choice for people looking to stay agile and reduce stiffness, especially if they have arthritis or other joint issues, Daibes explained.
Plus, the focus on deep breathing and mindfulness makes tai chi a great stress reliever, helping you unwind and find inner peace, he added.
ADVERTISING
Top ways to lower blood pressure
Besides tai chi, there are several other effective ways to lower blood pressure.
“Regular exercise, such as brisk walking or swimming, along with a healthy diet rich in fruits, vegetables, and whole grains, can make a significant difference for reducing blood pressure,” said Daibes. “Managing weight, reducing sodium intake, limiting alcohol consumption, quitting smoking, and prioritizing quality sleep are also essential steps.”
Stress management techniques like deep breathing exercises and meditation can help, as can medication when necessary. It’s crucial to find the right combination of lifestyle changes and medical interventions with the guidance of a healthcare provider for optimal results, Daibes added.
Also, the value of aerobic exercise in lowering blood pressure should not be overlooked.
“Moderate intensity aerobic exercise is considered the gold standard for exercise-based treatment of high blood pressure,” Petreycik explained. “Because of the recommended guidelines of 150 minutes or more per week, this considerable time commitment may be difficult for many to adhere to.”
There is a growing body of evidence showing a dose-response relationship between exercise intensity and blood pressure. Simply put, as the exercise intensity increases, one can expect a lower resting systolic and diastolic blood pressure, he explained.
People who are physically capable and have approval from their physician “to participate in high intensity interval training (HIIT), there is potential for reductions in blood pressure similar to that with taking commonly prescribed blood pressure medications,” said Petreycik. “Adapting to the higher intensity aerobic exercise improves cardiorespiratory fitness which has been shown to address common comorbidities related to high blood pressure, such as diabetes and obesity.”
From a dietary perspective, the heart-healthy Mediterranean Diet can help lower blood pressure with its emphasis on a rich variety of plant-based foods, protein sources low in saturated fat and cholesterol, and inclusion of unsaturated fats such as nuts, seeds, and oils, Petreycik stated.
Adhering to recommended guidelines for sodium intake can also help lower blood pressure. For most people, this may be consuming less than 2,300 mg per day. For others with preexisting health conditions, their doctor may recommend as little as 1500 mg per day.
The combination of a heart-healthy diet and exercise regimen can assist with weight loss or weight management. Losing as little as 10lbs if you are considered overweight or obese can have a positive impact on lowering blood pressure, Petreycik added.
Takeaway
According to a recent study, tai chi was more effective compared to aerobic exercise in lowering blood pressure among prehypertension patients.
There are many health benefits of tai chi, which include decreasing stress, boosting mood, and promoting heart health, all of which can help with hypertension.
Other ways to lower blood pressure include working out on a regular basis and eating a healthy diet rich in fruits, vegetables, and whole grains.


